
There is currently no commonly acceptable treatment to reverse the effects of dry AMD. Treatment with antioxidants and minerals may delay and possibly prevent intermediate dry AMD from progressing to the advanced stage. In addition, antioxidants and minerals significantly reduce the risk of the development of advanced AMD in the fellow eye of a patient with advanced AMD in their first eye.
For patients who do not have intermediate or advanced AMD, but have other risk factors for AMD such as a strong family history of AMD, we recommend lifestyle modifications which may slow AMD progression:
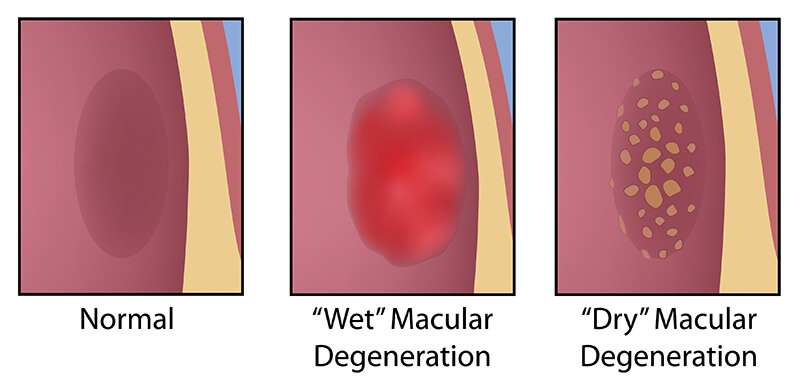
Neovascular AMD also called Wet AMD needs to be treated as soon as possible after it is diagnosed, to prevent more severe, irretrievable vision loss. The location of the abnormal blood vessels in wet AMD will determine treatment options. For more information go to Eyesight’s Macular Degeneration Center page.
If the abnormal blood vessels beneath the retina are not under or adjacent to the fovea (the very center of the macula), then laser photocoagulation is an option. This type of laser treatment will destroy the abnormal blood vessels beneath the retina, sealing off leakage and bleeding. Because the heat of this laser treatment also destroys the overlying healthy retina tissue, a permanent blind spot will result wherever the laser is applied. Hence, if the laser is used to treat abnormal vessels beneath the center of the macula, the patient will have a permanent blind spot in the most important area of the macula, the very part that we most want saved. In addition, approximately half of all patients treated with laser photocoagulation will require retreatment, resulting in the creation of an even larger blind spot.
When the abnormal blood vessels are in or adjacent to the center of the macula, photodynamic therapy (PDT) with Visudyne is now available.
Visudyne is a light-activated drug which is injected into the bloodstream. As the drug travels through the blood, it preferentially collects in the abnormal blood vessels under the retina. A non-thermal, low power laser (that does not burn the retina) is used to activate the Visudyne which then causes closure of the abnormal blood vessels without damaging the overlying retina, which we are trying to preserve.
Visudyne therapy, when used alone, is usually a multi-course treatment. It is unusual to permanently close off the abnormal blood vessels or prevent further leakage from them with just one or two treatments.
Because of the aggressive nature of the disease, multiple Visudyne treatments (at up to three month intervals) may be necessary. A typical treatment schedule is three to four treatments in the first year, with about half as many needed in the second and possibly third years.
Though Visudyne therapy cannot restore vision which is already lost, its major benefit is slowing or preventing the progression of vision loss through AMD. This vision loss has been shown to be significantly less than with standard laser photocoagulation or no treatment at all.
Our practice is proud to offer Eylea for the treatment of retina disease. Eyelea works by preventing new blood vessels from forming under the retina (the inside back of the eye). In people with a certain type of eye disease, new blood vessels grow under the retina where they leak blood and fluid. This is known as the “wet form” of macular degeneration.
Eylea is an injection used to treat swelling in the retina caused by blockage in the blood vessels. It is also used to treat the following vision threatening eye conditions:
There is compelling evidence in the literature that the use of intravitreal steroids is helpful in the treatment of wet AMD. This class of medications has been shown to reduce inflammation in the retina, decrease leakage or edema, and may inhibit the stimulus for growth of the abnormal blood vessels in wet AMD. Both triamcinolone acetonide and dexamethasone have shown positive results when used concurrently with PDT and Visudyne.
In February of 2005, the first of a new category of drugs to treat wet macular degeneration was released. These drugs fall into the realm of anti-angiogenic therapy, inhibiting the growth of the new blood vessels beneath the retina that are the source of the damaging fluid and blood which destroys the overlying healthy retina.
The first of these anti-angiogenic drugs is Macugen. This is a novel medication, an RNA molecule that blocks the signal for new blood vessel growth.
Avastin and Lucentis are more potent anti-vascular endothelial growth factor (anti-VEGF) drugs. Both are monoclonal antibodies to the VEGF molecule. Avastin was released by the FDA in 2000 for the inhibition of new blood vessel growth in tumors from colon cancer, breast cancer and some forms of lung cancer. In late 2005 it was adopted for “off-label” use via intravitreal injection for the treatment of abnormal blood vessel growth in wet AMD. Lucentis was released in the second half of 2006 for similar use. Most ophthalmologists treating macular degeneration believe both Avastin and Lucentis give similar results, however this is yet to be proven.
All intravitreal drugs are administered directly into the eye in a relatively quick and pain-free manner. When used as monotherapy, intravitreal anti-VEGF medications need to be administered fairly often (Lucentis every 4 weeks, Macugen every 6 weeks, Avastin every 4-6 weeks).
Combination therapies are useful to attack diseases from multiple different “directions.” This also appears to be true with treating wet AMD.
Using combinations of multiple different treatments may result in fewer treatments being necessary, fewer or less significant side effects, lower costs, and perhaps higher degrees of success.